PM-JAY / Ayushman Bharth Health Card
Outline for NHA under PM-JAY / Ayushman Bharth Health Card
Introduction
- What is NHA?
- What is PM-JAY?
- Objectives of PM-JAY
- Role of NHA in PM-JAY
Key features of PM-JAY
- Eligibility
- Benefits
- Coverage
- Cashless and paperless access
- Portability
III. NHA’s implementation and oversight of PM-JAY
- Developing and implementing policies and guidelines
- Empaneling hospitals
- Providing financial assistance to states
- Monitoring and evaluating the scheme
- Addressing fraud and abuse
-
Achievements of PM-JAY
- Number of beneficiaries enrolled
- Number of claims processed
- Amount of claims paid
- Impact on access to healthcare
- Impact on financial protection
Challenges and opportunities
- Challenges:
- Raising awareness among beneficiaries
- Ensuring quality of care in empanelled hospitals
- Preventing fraud and abuse
- Opportunities:
- Expanding coverage to more beneficiaries
- Integrating with other healthcare schemes
- Using technology to improve efficiency and transparency
Introduction

What is NHA?
The National Health Authority (NHA) is an autonomous agency under the Ministry of Health and Family Welfare, Government of India. It is responsible for the implementation and management of the Pradhan Mantri Jan Arogya Yojana (PM-JAY), the world’s largest health insurance/assurance scheme.
What is PM-JAY?
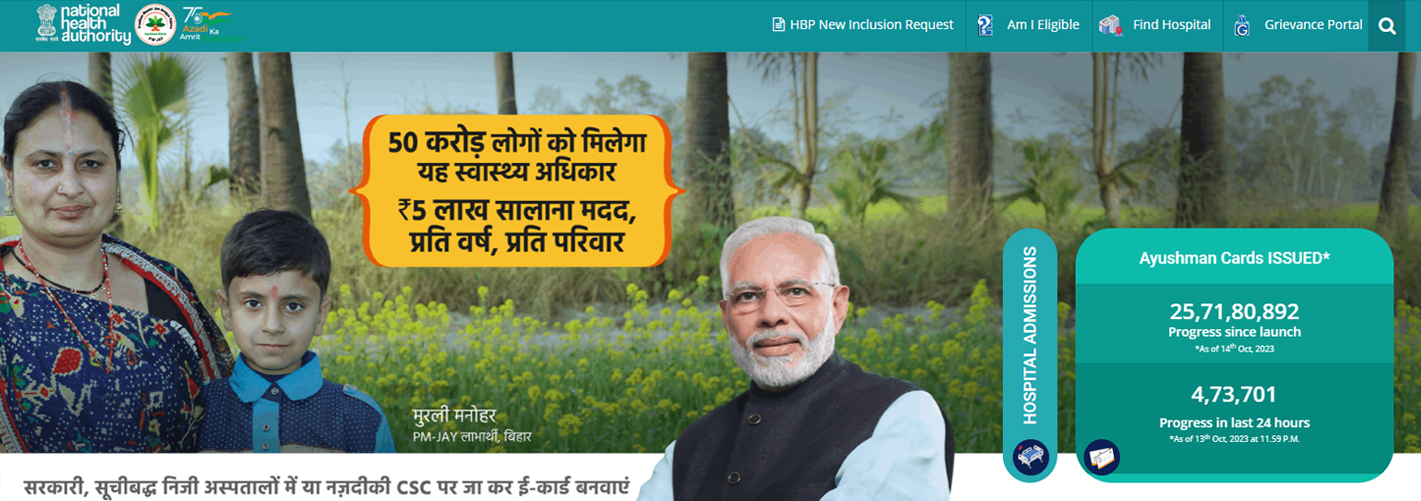
Pradhan Mantri Jan Arogya Yojana (PM-JAY), also known as Ayushman Bharat Yojana, is a flagship scheme of the Government of India that provides free secondary and tertiary care hospitalization to eligible beneficiaries. The scheme covers over 12 crore poor and vulnerable families (approximately 55 crore beneficiaries) across India.
Objectives of PM-JAY
The objectives of PM-JAY are to:
- Provide financial protection to poor and vulnerable families from the high cost of hospitalization
- Improve access to quality healthcare services
- Reduce out-of-pocket expenditure on healthcare
- Promote equity in healthcare
Role of NHA in PM-JAY
NHA plays a pivotal role in the implementation and management of PM-JAY. Its key responsibilities include:
- Developing and implementing policies and guidelines for PM-JAY
- Empaneling hospitals
- Providing financial assistance to states
- Monitoring and evaluating the scheme
- Addressing fraud and abuse
NHA also works closely with state governments to ensure the smooth implementation of PM-JAY at the state level.
In addition to the above, NHA also plays a key role in:
- Raising awareness about PM-JAY among beneficiaries
- Educating beneficiaries about their rights and entitlements under the scheme
- Resolving beneficiary grievances
- Promoting quality of care in empanelled hospitals
NHA is committed to making PM-JAY a success and achieving its objectives of providing financial protection and access to quality healthcare services to all eligible beneficiaries.

Key features of PM-JAY
Eligibility
PM-JAY is open to all poor and vulnerable families who are identified as eligible based on the Socio-Economic Caste Census (SECC) 2011 data. There is no restriction on family size, age, or gender.
Benefits
PM-JAY provides a cover of Rs. 5 lakhs per family per year for secondary and tertiary care hospitalization across public and private impanelled hospitals in India. The scheme covers a wide range of medical procedures and treatments, including:
- Medical examination, treatment, and consultation
- Pre-hospitalization and post-hospitalization expenses
- Medicines and medical consumables
- Non-intensive and intensive care services
- Diagnostic and laboratory investigations
Coverage
PM-JAY provides nationwide coverage. Beneficiaries can avail of cashless treatment at any impaneled hospital across India.
Cashless and paperless access
PM-JAY provides cashless and paperless access to healthcare services. Beneficiaries can simply present their Ayushman Bharat Card at the impaneled hospital to avail of treatment. The hospital will directly settle the claim with NHA.
Portability
The benefits of PM-JAY are portable across India. This means that a beneficiary from one state can avail of benefits at any impaneled hospital in another state.
Key benefits of PM-JAY
- PM-JAY provides free secondary and tertiary care hospitalization to eligible beneficiaries.
- The scheme covers a wide range of medical procedures and treatments.
- PM-JAY provides nationwide coverage.
- Beneficiaries can avail of cashless and paperless treatment at any impanelled hospital across India.
- The benefits of PM-JAY are portable across India.
PM-JAY has made a significant impact on the lives of millions of poor and vulnerable families in India. The scheme has provided them with access to quality healthcare services that they would otherwise not have been able to afford.
III. NHA’s implementation and oversight of PM-JAY
Developing and implementing policies and guidelines
NHA is responsible for developing and implementing policies and guidelines for PM-JAY. These policies and guidelines cover a wide range of areas, such as:
- Eligibility criteria
- Benefits covered
- Claim processing procedures
- Hospital empanelment process
- Fraud prevention and detection
NHA also develops and maintains the PM-JAY portal, which is a one-stop shop for all stakeholders, including beneficiaries, hospitals, and state governments. The portal provides information on the scheme, as well as facilities for beneficiary registration, hospital empanelment, and claim processing.
Empaneling hospitals
NHA is responsible for empaneling hospitals under PM-JAY. Hospitals are impaneled through a transparent and objective process. Impaneled hospitals must meet certain quality standards and agree to provide cashless and paperless treatment to PM-JAY beneficiaries.
Providing financial assistance to states
NHA provides financial assistance to states for the implementation of PM-JAY. The financial assistance is provided on the basis of the number of eligible beneficiaries in each state and the cost of hospitalization services in the state.
Monitoring and evaluating the scheme
NHA monitors and evaluates the implementation of PM-JAY on a regular basis. This includes tracking the number of beneficiaries enrolled, the number of claims processed, the number of claims paid, and the quality of care provided by impaneled hospitals. NHA also conducts surveys and interviews with beneficiaries to get their feedback on the scheme.
Addressing fraud and abuse
NHA has a zero-tolerance policy towards fraud and abuse under PM-JAY. NHA has set up a National Anti-Fraud Unit (NAFU) to investigate and prevent fraud and abuse under the scheme. NAFU works closely with state anti-fraud units and impanelled hospitals to identify and address fraudulent activities.
NHA’s implementation and oversight of PM-JAY is critical to the success of the scheme. NHA’s efforts have helped to ensure that PM-JAY is implemented in a transparent and efficient manner and that beneficiaries are able to avail the benefits of the scheme without any hassle.
Additional measures taken by NHA to ensure the smooth implementation of PM-JAY
- NHA provides capacity-building training to state government officials and hospital staff on the implementation of PM-JAY.
- NHA has developed a robust IT system to support the implementation of PM-JAY. The system enables real-time tracking of beneficiary registrations, hospital empanelment, and claim processing.
- NHA has a dedicated call center to resolve beneficiary grievances.
- NHA conducts regular audits of impanelled hospitals to ensure compliance with the scheme’s guidelines.
NHA is committed to making PM-JAY a success and achieving its objectives of providing financial protection and access to quality healthcare services to all eligible beneficiaries.
Achievements of PM-JAY
https://www.youtube.com/watch?v=mrv6HmCl4S4
Number of beneficiaries enrolled
Over 15.5 crore families (about 50 crore beneficiaries) have been enrolled in PM-JAY since its launch in 2018. This makes PM-JAY the world’s largest health insurance/assurance scheme.
Number of claims processed
Over 5.39 crore claims have been processed under PM-JAY as of March 2023. This is a testament to the scale and reach of the scheme.
Amount of claims paid
Over Rs. 66,284 crores has been paid to impanelled hospitals under PM-JAY as of March 2023. This has helped to reduce the financial burden on poor and vulnerable families.
Impact on access to healthcare
PM-JAY has had a significant impact on access to healthcare for poor and vulnerable families. The scheme has enabled them to avail quality healthcare services that they would otherwise not have been able to afford.
Impact on financial protection
PM-JAY has provided financial protection to poor and vulnerable families from the high cost of hospitalization. The scheme has reduced their out-of-pocket expenditure on healthcare by up to 60%.
The overall impact of PM-JAY
PM-JAY has made a significant impact on the lives of millions of poor and vulnerable families in India. The scheme has provided them with access to quality healthcare services and financial protection from the high cost of hospitalization. PM-JAY has played a key role in improving the health and well-being of the Indian population.
Additional achievements of PM-JAY
- PM-JAY has reduced the number of people who are forced to sell their assets or borrow money to pay for hospitalization.
- PM-JAY has increased the utilization of healthcare services by poor and vulnerable families.
- PM-JAY has improved the quality of care provided by impanelled hospitals.
- PM-JAY has helped to reduce the regional disparities in access to healthcare.
PM-JAY is a flagship scheme of the Government of India that is making a real difference in the lives of millions of people. The scheme is a testament to the government’s commitment to providing universal healthcare to all citizens.
Challenges and opportunities
Challenges
- Raising awareness among beneficiaries: Many eligible beneficiaries are not aware of the PM-JAY scheme or its benefits. NHA is working to raise awareness through various initiatives, such as public awareness campaigns and capacity-building training for state government officials and hospital staff.
- Ensuring quality of care in impaneled hospitals: NHA has put in place various measures to ensure the quality of care in impaneled hospitals, such as developing and implementing quality standards, conducting regular audits, and establishing a grievance redressal mechanism. However, there are still some challenges that need to be addressed, such as inadequate infrastructure and human resources in some hospitals.
- Preventing fraud and abuse: NHA has a zero-tolerance policy towards fraud and abuse under PM-JAY. However, fraud and abuse is a challenge that all health insurance schemes face. NHA is working to prevent fraud and abuse by developing and implementing anti-fraud measures, such as risk-based audits and data analytics.
Opportunities
- Expanding coverage to more beneficiaries: PM-JAY currently covers over 15.5 crore families (about 50 crore beneficiaries). However, there are still some eligible families who are not covered by the scheme. NHA is working to expand coverage to more beneficiaries by identifying and enrolling them in the scheme.
- Integrating with other healthcare schemes: NHA is working to integrate PM-JAY with other healthcare schemes, such as the Rashtriya Swasthya Bima Yojana (RSBY) and the Chief Minister’s Arogya Bima Yojana (CMABY). This will make it easier for beneficiaries to avail the benefits of all healthcare schemes seamlessly.
- Using technology to improve efficiency and transparency: NHA is using technology to improve the efficiency and transparency of PM-JAY. For example, NHA has developed a mobile app for beneficiaries to track their enrollment status, view their benefits, and file claims. NHA is also using data analytics to identify and address fraud and abuse.
NHA is committed to addressing the challenges and seizing the opportunities to make PM-JAY a success. The scheme has the potential to transform the healthcare landscape of India by providing universal health coverage to all citizens.
- Conclusion
The role of NHA under PM-JAY is critical to the successful implementation of the scheme. NHA is responsible for developing and implementing policies and guidelines, empaneling hospitals, providing financial assistance to states, monitoring and evaluating the scheme, and addressing fraud and abuse.
PM-JAY has made significant progress since its launch in 2018. Millions of beneficiaries have been enrolled in the scheme and millions of claims have been processed. The scheme has positively impacted access to healthcare and financial protection for the poor and those in need of special care, support, or protection because of age, disability, or risk.
There are still some challenges that need to be addressed, such as raising awareness among beneficiaries, ensuring the quality of care in impaneled hospitals, and preventing fraud and abuse. However, the opportunities for PM-JAY are immense. With NHA’s continued efforts, the scheme can be expanded to cover more beneficiaries and integrated with other healthcare schemes. Technology can also be used to improve the efficiency and transparency of the scheme.